Anal fissures are small tears in the lining of the anus, causing pain and discomfort. They can occur due to various reasons, including straining during bowel movements. The duration of an anal fissure can vary; while some fissures heal within a few weeks with proper care, others may persist and require medical or surgical intervention.
If an anal fissure does not improve within a few weeks, it’s essential to seek medical advice. Persistent fissures can lead to chronic pain and complications. It’s important to address symptoms early to avoid long-term discomfort and other issues.

Symptoms
- Worst Symptoms of Anal Fissures
- Sharp knife-like pain during bowel movements
- Bleeding
- Visible tear near the anus and may also have an external skin tag
- Symptoms Distinguishing Internal from External Anal Fissures
- Internal fissures: Occur inside the anal canal, may not be visible
- External fissures: Located at the anal opening, visible as small cuts
- Early Signs of Anal Fissures
- Itching
- Mild discomfort
- Tenderness around the anus
Causes and Risk Factors
- Common Causes of Anal Fissures
- Straining during bowel movements
- Passing hard stools
- Chronic constipation or diarrhea
- Can Anal Fissures Heal on Their Own?
- Mild cases can heal with proper care and lifestyle changes
- Is it Okay to Live with Anal Fissures?
- Managing mild symptoms is possible, but seeking treatment is recommended to avoid complications
Treatment Options for Anal Fissure
Anal fissures can be categorized into two types: acute and chronic. Acute fissures are recent and may heal with conservative treatments, while chronic fissures have been present for longer and may require surgical intervention.
Lateral Internal Sphincterotomy (LIS)
Lateral Internal Sphincterotomy (LIS) is a surgical procedure for treating chronic anal fissures. It involves a small incision in the internal anal sphincter muscle to reduce spasms and alleviate pain, promoting fissure healing. LIS is highly effective for chronic cases that do not respond to conservative treatments.
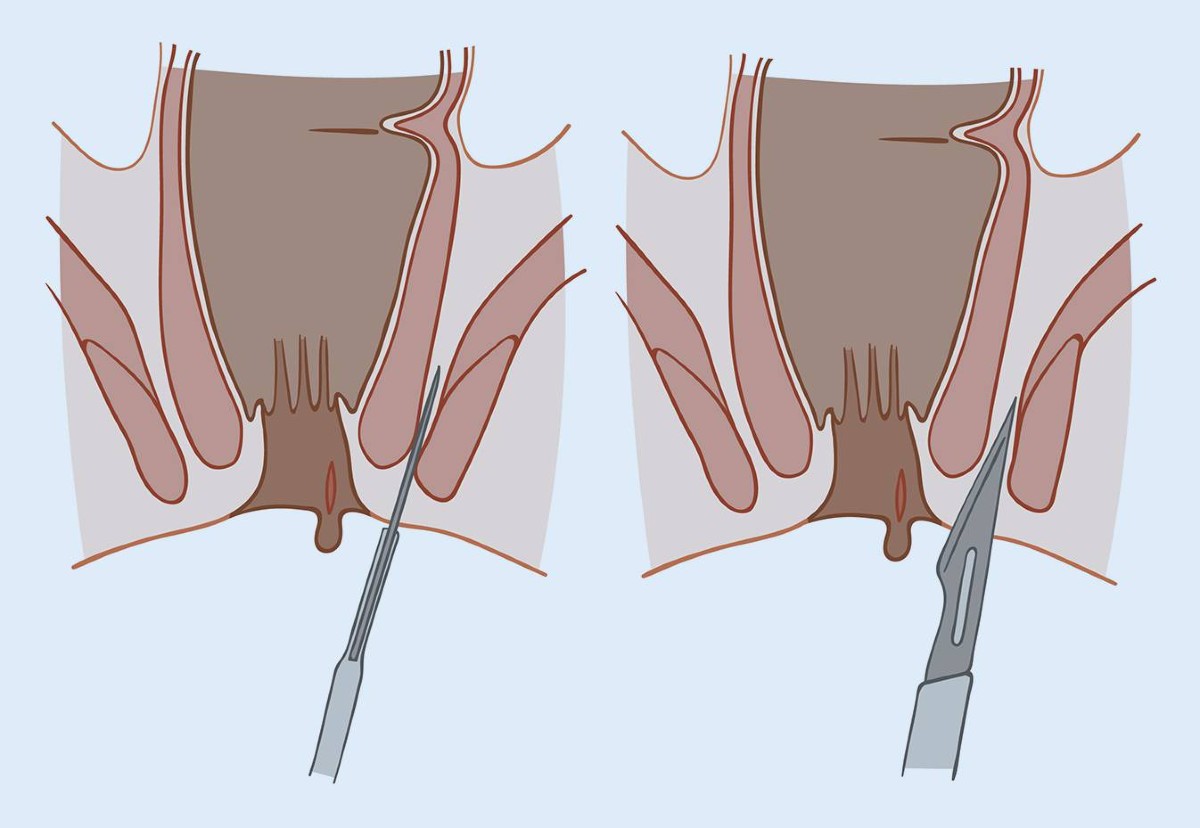
Performed under local or general anesthesia, LIS involves making a small cut in the internal anal sphincter, reducing muscle tension and improving blood flow for accelerated healing. The minimally invasive procedure is typically done on an outpatient basis, allowing the patient to return home the same day.
- Effective Relief: LIS provides lasting relief for chronic fissures, particularly when other treatments have failed.
- Minimal Pain: The procedure reduces muscle spasms, significantly decreasing fissure-related pain.
- Outpatient Procedure: Patients can go home the same day, ensuring minimal disruption to daily life.
Quick Recovery: Most individuals resume regular activities within a few days.
Recovery from LIS is relatively quick. Most patients resume normal activities within a few days, with complete healing taking a few weeks. Minor discomfort may occur post-surgery but gradually subsides as healing progresses. Proper post-operative care, such as maintaining stool softness and hygiene, supports optimal recovery.
Special Considerations
Sleeping on your side or stomach can reduce pressure on the anal area, helping to alleviate pain from a fissure.
A fissure at the 6 o'clock position refers to the location of the tear, typically at the back of the anal canal.
Common Misconceptions
Vaseline can provide temporary relief by reducing friction, but it is not a treatment for healing fissures. Consult a healthcare provider for appropriate treatment options.
Bananas are high in fiber and can help soften stools, making them beneficial for preventing and managing fissures.
Popcorn can be difficult to digest and may irritate the digestive tract, potentially worsening fissure symptoms.
Coffee can cause dehydration and hard stools, which may exacerbate fissures. Staying hydrated and limiting caffeine intake can help.
Ibuprofen can help reduce pain and inflammation but does not treat the underlying fissure. Consult a healthcare provider for appropriate treatments.
Frequently Asked Questions (FAQs)
Hemorrhoids are swollen veins in the rectum or anus, while fissures are small tears in the anal lining. Hemorrhoids often cause bleeding and itching, while fissures cause sharp pain during bowel movements.
Avoid straining during bowel movements, and refrain from using harsh toilet paper. Maintain good hygiene and avoid irritants.
To poop comfortably, use a stool to elevate your feet, which can help align the rectum and reduce strain. Ensure your stool is soft by staying hydrated and eating a fiber-rich diet.
Massaging a fissure is not recommended as it can cause further irritation and delay healing.
Persistent fissures may not heal due to continued strain, infection, or underlying conditions that require medical evaluation.
This might indicate a prolapsed hemorrhoid or other condition. Consult a healthcare provider for a proper diagnosis.
Yes, a healthcare provider can typically diagnose a fissure through a physical examination.
Chronic fissures can lead to the development of fistulas, which are abnormal connections between the anal canal and the skin.
A fissure is a tear in the anal lining, while a fistula is an abnormal connection. Symptoms of a fistula include persistent pain, swelling, and discharge. A healthcare provider can diagnose the condition.
The beginning of a fistula may feel like a tender, swollen area near the anus, often accompanied by pain and drainage.
Fistula discharge can vary in color but is often yellow or white due to pus.
Conditions such as abscesses, hidradenitis suppurativa, and pilonidal cysts can mimic fistulas.
Persistent pain, swelling, and drainage near the anus may indicate a fistula. However, a proper diagnosis requires a medical evaluation.
Submit your Suggestion





