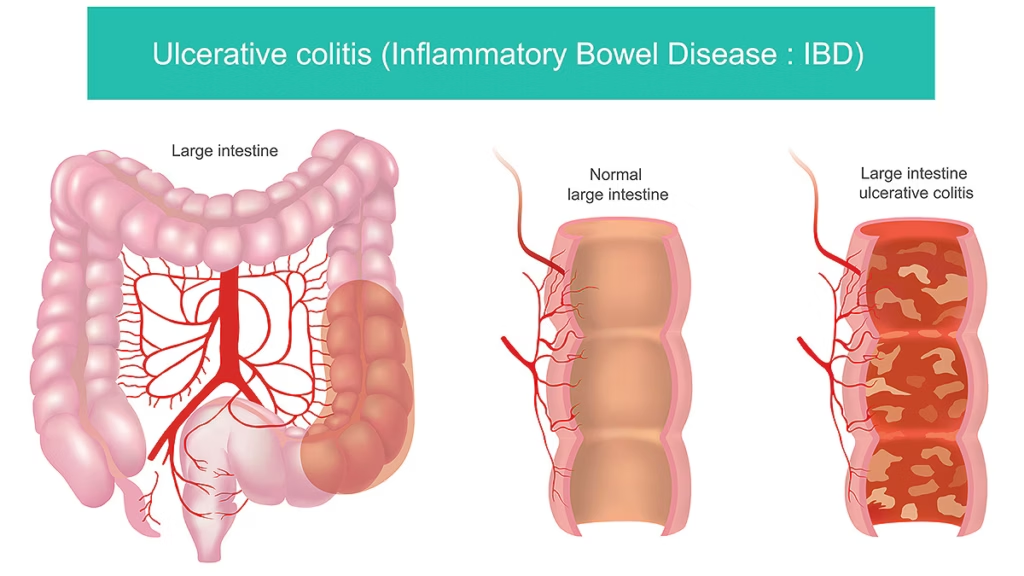
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the lining of the colon and rectum. It causes ulcers, inflammation, and irritation, leading to symptoms like diarrhea, abdominal pain, and rectal bleeding. Unlike other digestive conditions, ulcerative colitis is an autoimmune disorder, meaning the body mistakenly attacks the colon’s lining.
How Serious is Ulcerative Colitis?
UC can range from mild to severe, with symptoms that may flare up unpredictably. While some people experience periods of remission, others may struggle with persistent symptoms that impact daily life. In severe cases, complications like colon perforation, toxic megacolon, or an increased risk of colorectal cancer can develop.
Does Ulcerative Colitis Ever Go Away?
Unfortunately, there is no permanent cure for ulcerative colitis. However, with proper treatment, lifestyle adjustments, and medication, many individuals can achieve long-term remission, reducing or even eliminating symptoms for extended periods.
What is End-Stage Ulcerative Colitis?
End-stage ulcerative colitis, also known as fulminant colitis, is the most severe form of the disease, where inflammation spreads rapidly and can lead to life-threatening complications. In such cases, surgery, including a colectomy (removal of the colon), may be necessary.
What are the Four Stages of Ulcerative Colitis?
- Mild UC: Occasional diarrhea with mild pain and little to no blood in the stool.
- Moderate UC: More frequent bowel movements with noticeable blood, abdominal discomfort, and fatigue.
- Severe UC: Intense abdominal pain, frequent diarrhea with heavy bleeding, weight loss, and fever.
- Fulminant UC: A rare but life-threatening stage requiring immediate medical intervention, often leading to surgery.
Is There a Difference Between Colitis and Ulcerative Colitis?
Yes. Colitis is a general term for inflammation of the colon, which can be caused by infections, medications, or other factors. Ulcerative colitis, on the other hand, is a chronic autoimmune disease that specifically affects the colon lining and requires long-term management.
Identification and Symptoms
What Does Colitis Poop Look Like?
Stools in ulcerative colitis can vary but often appear loose, bloody, or contain mucus. Some individuals experience explosive diarrhea, while others may have pencil-thin stools due to inflammation.
Where is Colitis Pain Felt?
Pain is typically felt in the lower left abdomen but can extend throughout the belly. It is often described as cramping, sharp pain, or a persistent ache that worsens before bowel movements.
What Are the Signs of Worsening Ulcerative Colitis?
- Increased frequency and urgency of bowel movements
- More severe rectal bleeding
- Intense abdominal cramping
- Sudden weight loss
- Persistent fever or extreme fatigue
Do You Always Bleed with Ulcerative Colitis?
Not necessarily. While rectal bleeding is a common symptom, some individuals may experience UC without noticeable blood in their stool. However, inflammation and irritation in the colon can still cause discomfort and urgency.
Can You Get Sepsis from Ulcerative Colitis?
Yes. If severe inflammation leads to perforation (a hole in the colon) or toxic megacolon (life-threatening colon dilation), bacteria can enter the bloodstream, causing sepsis—a serious, potentially fatal condition.
How Many Bowel Movements Should You Have with Ulcerative Colitis?
Bowel movements vary by severity. Mild cases may involve 2-4 trips per day, while severe flare-ups can cause 10+ urgent, watery stools within 24 hours.
Causes
Ulcerative colitis develops due to a combination of genetic, immune system, and environmental factors. While the exact cause remains unknown, researchers believe that an overactive immune response mistakenly attacks the colon lining, triggering inflammation.
Triggers and Risk Factors
- Genetics – A family history of inflammatory bowel disease (IBD) increases the likelihood of developing UC.
- Immune System Dysfunction – UC occurs when the immune system misidentifies harmless bacteria in the gut as threats and launches an inflammatory response.
- Age – Most diagnoses occur between the ages of 15 and 30, though UC can develop at any age.
- Stress – Emotional or physical stress can exacerbate symptoms, though it is not a direct cause.
- Dietary Factors – While diet doesn’t cause UC, certain foods can worsen symptoms, particularly processed foods, dairy, and high-fat meals.
- Medications – Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can irritate the gut lining and trigger flare-ups.
- Smoking & Alcohol – Unlike Crohn’s disease, smoking may reduce UC symptoms in some cases, though the health risks outweigh potential benefits. Alcohol, however, can worsen inflammation.
Treatment Options for Ulcerative Colitis
Ulcerative colitis treatment aims to reduce inflammation, prevent flare-ups, and maintain long-term remission. Treatment plans vary based on severity, patient response, and lifestyle factors.
Colectomy (Colon Removal Surgery)
For individuals with severe ulcerative colitis (UC) that does not respond to medications or leads to life-threatening complications, colectomy (colon removal surgery) is considered a permanent solution. This surgical intervention eliminates the diseased colon and can restore quality of life for those struggling with chronic symptoms.
A colectomy involves the partial or total removal of the colon, depending on the severity of the disease. After the removal, surgeons create an alternative way for waste to exit the body, typically using one of the following techniques:
Total Colectomy with Ileostomy:
- The entire colon is removed, and a stoma (opening in the abdomen) is created.
- Waste exits the body through an external ileostomy bag, which collects stool.
Ileal Pouch-Anal Anastomosis (J-Pouch Surgery):
- The diseased colon and rectum are removed, but instead of using an external bag, a J-pouch is created from the small intestine.
- This allows waste to be eliminated through the anus, preserving more natural bowel function.
- J-pouch surgery is often performed in two or three stages to ensure proper healing.
Subtotal Colectomy:
- Only a portion of the colon is removed, typically in cases of less extensive disease.
- The remaining healthy colon is reconnected to preserve some normal function.
✅ Permanent cure for UC – Eliminates inflammation and symptoms.
✅ No more dependence on immunosuppressive medications – Reducing risks of long-term side effects.
✅ Prevents complications – Eliminates risks of toxic megacolon, colon cancer, and life-threatening infections.
✅ Improved quality of life – Restores the ability to eat freely and reduces debilitating flare-ups.
🔹 Hospital Stay: Typically 5 to 7 days post-surgery, depending on the procedure type.
🔹 Full Recovery: Can take weeks to months, with gradual adjustments to diet and activity.
🔹 Temporary or Permanent Lifestyle Changes: If an ileostomy is performed, patients must learn how to manage an ostomy bag.
🔹 Dietary Modifications: Initially, a low-fiber diet is recommended, with gradual reintroduction of fiber and solid foods.
🔹 J-Pouch Adaptation: Those who undergo J-pouch surgery may experience frequent bowel movements initially, but this improves over time.
Who Needs a Colectomy?
Surgery is recommended in the following situations:
- Severe, medication-resistant UC that does not improve with treatment.
- Life-threatening complications, such as toxic megacolon, perforation, or severe bleeding.
- Increased cancer risk – Chronic inflammation significantly raises the risk of colon cancer in long-standing UC patients.
- Steroid dependence or severe medication side effects impacting overall health.
Key Takeaway:
While a colectomy is a major surgery, it provides a definitive cure for ulcerative colitis, allowing patients to regain control over their health. The choice between ileostomy and J-pouch surgery depends on individual circumstances, and consulting a colorectal surgeon is crucial for determining the best approach.
Frequently Asked Questions (FAQs)
A healthy diet rich in fruits, vegetables, and whole grains can help maintain overall skin health and prevent conditions that may contribute to skin tags.
Professional treatments like cryotherapy, cauterization, and excision are effective methods for destroying skin tags.
Skin tag removal pens can be effective for some individuals, but results vary. It’s best to consult a healthcare provider for advice.
Losing weight can reduce friction and the likelihood of new skin tags forming, but existing skin tags typically do not go away on their own.
It is not recommended to remove skin tags overnight due to the risk of infection and improper healing.
Apple cider vinegar is a popular home remedy believed to dry out skin tags, causing them to fall off. However, it can cause skin irritation and should be used with caution.
Cutting off a skin tag with nail clippers is not recommended due to the risk of infection and improper healing. Always seek professional advice.
Tea tree oil is believed to dry out skin tags, but it can cause skin irritation. Use with caution and discontinue if irritation occurs.
Some believe that placing a banana peel on a skin tag overnight can help it fall off due to the peel’s enzymes, but there is limited scientific evidence to support this.
Hydrogen peroxide can help keep the area clean but is not a definitive treatment for removing skin tags.
Dr. Scholl’s Freeze Away is designed for warts but may also be used on skin tags. Consult a healthcare provider before use.
Applying clear fingernail polish to skin tags is a common home remedy believed to suffocate the tag, but it is not medically recommended.
Submit your Suggestion





