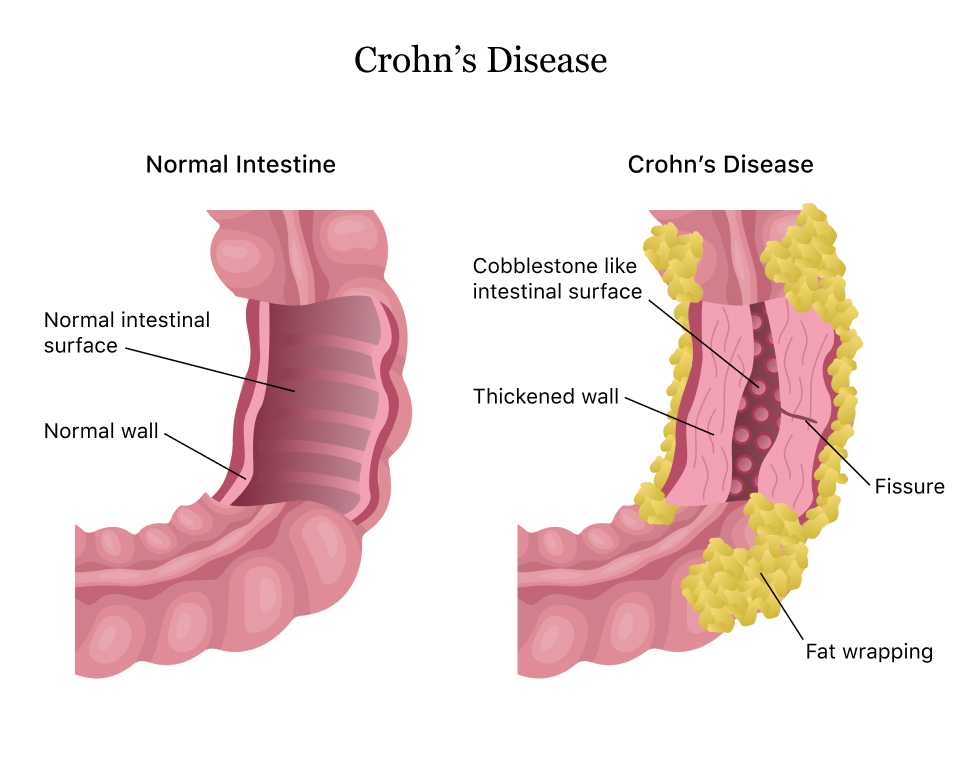
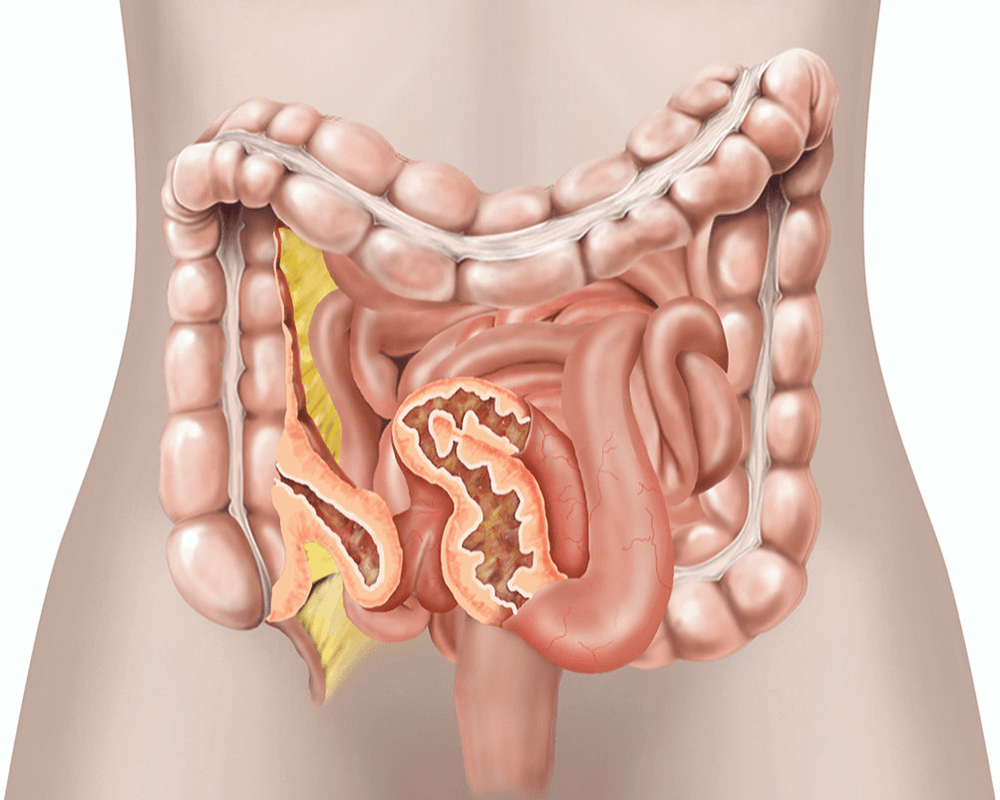
Crohn’s disease is a chronic inflammatory condition of the gastrointestinal (GI) tract, part of a group of conditions known as inflammatory bowel disease (IBD). It can affect any part of the GI tract from the mouth to the anus, but it most commonly affects the end of the small intestine and the beginning of the colon. When you have Crohn’s disease, your immune system attacks the GI tract, causing inflammation, pain, and damage. This can lead to a variety of symptoms, including abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition.
A condition known as “Crohn’s belly” refers to the abdominal distension and discomfort that many patients experience. “Creeping fat” is a phenomenon where fat wraps around the intestines, often observed in people with Crohn’s. Silent Crohn’s refers to periods when the disease is present without noticeable symptoms, making it difficult to diagnose and monitor. The life expectancy of someone with Crohn’s disease is generally normal with proper management, though the disease can significantly impact quality of life.
Crohn’s is recognized as a disability under the Americans with Disabilities Act (ADA) due to its impact on daily functioning. End-stage Crohn’s disease involves severe complications such as fistulas, strictures, and malnutrition. The worst outcomes of untreated Crohn’s can include life-threatening complications, making early and effective treatment crucial.
Symptoms and Diagnosis
What Does a Crohn’s Flare Feel Like?
- Intense abdominal pain or cramping
- Severe diarrhea
- Fatigue
- Nausea and vomiting
First Signs of Crohn’s:
- Persistent diarrhea
- Abdominal pain
- Blood in the stool
- Unexplained weight loss
- Fatigue
Sneaky Signs of Crohn’s Disease:
- Minor abdominal discomfort
- Frequent bowel movements
- Low-grade fever
- Anemia
- Joint pain
Indicators of Worsening Crohn’s:
- Increased frequency and severity of symptoms
- New or worsening abdominal pain
- Frequent, urgent bowel movements
- Blood in the stool
- Unintended weight loss
Pain and Fatigue:
- Crohn’s pain is usually felt in the lower right abdomen but can occur anywhere in the digestive tract.
- Crohn’s fatigue can be overwhelming, leading to increased sleep needs.
Bowel Movements and Daily Impact:
- Bowel movements with Crohn’s disease can vary but often include diarrhea and blood.
- People with Crohn’s may have frequent bowel movements, often more than six times a day.
- Symptoms can be worse in the morning.
Other Symptoms:
- Dizziness can occur, especially during flares due to dehydration or anemia.
- Hunger can be affected; some may lose appetite while others may experience increased hunger.
Causes and Risk Factors
What Causes Crohn’s Disease?
- The exact cause is unknown, but it involves a combination of genetic, environmental, and immune system factors.
- Common triggers include stress, smoking, and certain medications.
Common Misdiagnoses:
- Conditions such as irritable bowel syndrome (IBS), celiac disease, and infections can mimic Crohn’s symptoms.
Health Impacts:
- People with Crohn’s disease may get sick more easily due to a weakened immune system.
- The most common cause of death in Crohn’s disease is complications such as bowel obstruction, fistulas, or severe infection.
Treatment Options for Crohn’s Disease
Dietary Changes
Adopting a low-residue or low-fiber diet during flares to reduce symptoms, and incorporating a high-fiber diet during remission to support overall digestive health. Specific dietary adjustments may include avoiding certain trigger foods and incorporating supplements like ColoFlax to support gut health.
:max_bytes(150000):strip_icc()/myplate-balanced-diet-food-GettyImages-168340083-6cca166365b24954bafe82c2b7341262.jpg)
Helps manage symptoms, improve overall digestive health, and prevent flare-ups. Dietary changes can reduce inflammation, promote healing, and maintain remission.
Dietary adjustments can provide symptom relief within a few weeks, but ongoing adherence is necessary for long-term management.
Medications
Use of anti-inflammatory drugs, immune system suppressors, antibiotics, and biologics. Anti-inflammatory drugs like corticosteroids reduce inflammation, while immune system suppressors like azathioprine help control the immune response. Biologics, such as infliximab, target specific proteins involved in inflammation. It is important to get the right medicine for you so Consult Dr. Farooq before you lean towards this treatment option.

Reduces inflammation, controls the immune response, and helps prevent flare-ups. Medications can significantly improve quality of life and maintain long-term remission.
Varies; symptom improvement can be seen within weeks to months, depending on the medication and individual response.
Resection
Removal of the diseased segment of the intestine. The surgeon removes the affected area and reconnects the healthy ends of the intestine to restore normal bowel function.
Provides relief from symptoms when medication is not effective. Resection can eliminate the source of inflammation and improve overall health.
Recovery typically takes a few weeks, with hospital stays of about 5-10 days. Full recovery includes gradual return to normal activities and follow-up care to monitor for recurrence.
Strictureplasty
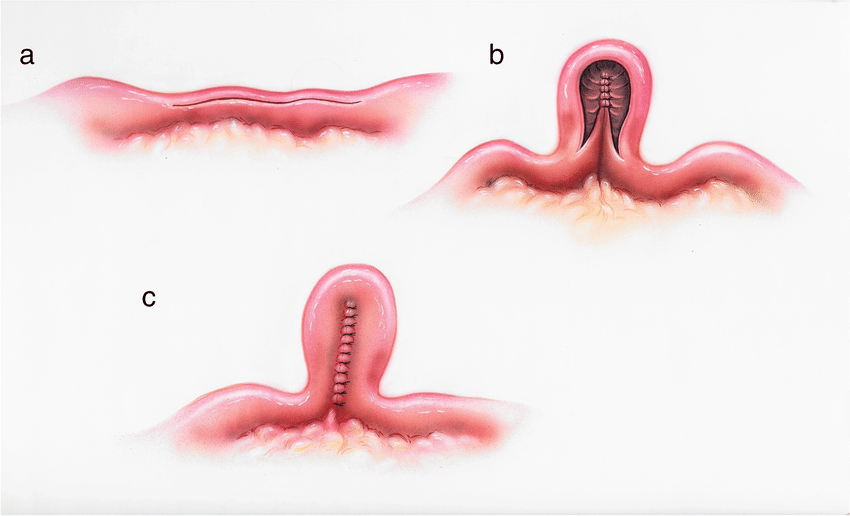
Widens narrowed areas of the intestine without removing any part. The surgeon makes an incision along the narrowed section and reshapes it to improve the passage of intestinal contents.
Maintains bowel length and function while relieving symptoms caused by strictures. Strictureplasty can prevent the need for more extensive surgery.
Recovery is similar to resection, with a few weeks for full recovery and hospital stays typically around 5-7 days.
Fistula Repair
Surgical closure of abnormal connections (fistulas) between the intestine and other organs or tissues. The surgeon removes the fistula and repairs the affected areas to restore normal function.
Eliminates the source of infection and inflammation, improving overall health and quality of life. Fistula repair can prevent recurrent infections and complications.
Recovery varies depending on the location and complexity of the fistula, but typically involves several weeks for full healing and close monitoring during recovery.
Frequently Asked Questions (FAQs)
Life expectancy is generally normal with proper management, though quality of life can be impacted.
Yes, it is recognized as a disability under the Americans with Disabilities Act (ADA).
End-stage Crohn’s involves severe complications like fistulas, strictures, and malnutrition.
Intense abdominal pain, severe diarrhea, fatigue, and nausea.
Weight gain can occur, but it is less common than weight loss due to malabsorption.
Persistent diarrhea, abdominal pain, blood in the stool, unexplained weight loss, and fatigue.
Often more than six times a day, especially during flares.
Symptoms can be worse in the morning.
Yes, dizziness can occur, especially during flares due to dehydration or anemia.
Acetaminophen is preferred over NSAIDs.
Dairy, high-fiber foods, spicy foods, and certain processed foods.
Easily digestible foods like bananas, rice, applesauce, and toast.
Submit your Suggestion





