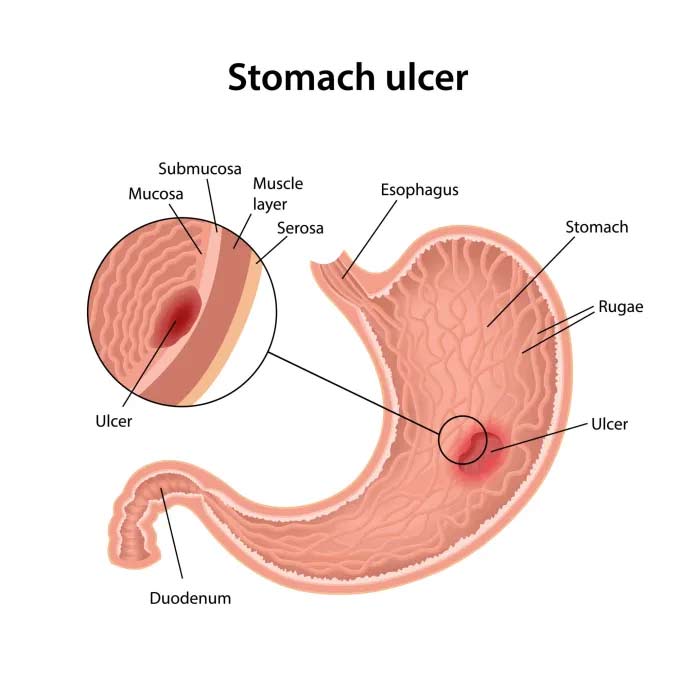
Stomach ulcers, also known as peptic ulcers, are open sores that develop on the lining of the stomach, small intestine, or esophagus. They are a common condition affecting millions of people worldwide. The difference between a stomach ulcer and a peptic ulcer is that peptic ulcers include both gastric (stomach) and duodenal (upper small intestine) ulcers. The primary cause of peptic ulcers is an infection with the bacterium Helicobacter pylori (H. pylori) or the long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs).
The number one cause of stomach ulcers is H. pylori infection, responsible for about 90% of all cases. Stomach ulcers can occur at any age, but they are more common in adults over the age of 50. Without treatment, stomach ulcers can lead to severe complications such as bleeding, perforation, and obstruction.
Symptoms
Warning Signs of Stomach Ulcers:
- Burning stomach pain
- Feeling of fullness, bloating, or belching
- Intolerance to fatty foods
- Heartburn
- Nausea
Symptoms of H. pylori:
- Abdominal pain or discomfort
- Frequent burping
- Loss of appetite
- Unintentional weight loss
- Bloating
Worst Symptoms of H. pylori:
- Severe abdominal pain
- Persistent nausea and vomiting
- Dark or tarry stools (indicating bleeding)
- Fatigue
Pain Location and Sensation:
- Peptic ulcer pain is typically felt in the upper abdomen and can be described as burning or gnawing.
- Ulcer pain may be constant or intermittent and can worsen on an empty stomach or at night.
Diagnostic Methods:
- Blood tests can detect H. pylori infection.
- Stool tests can identify H. pylori antigens.
- Breath tests measure carbon isotopes after ingesting a urea solution.
- Endoscopy allows direct visualization of the ulcer.
- CT scans can detect complications like perforations but are not the primary diagnostic tool.
Mimicking Conditions:
- Conditions such as pancreatitis, gastritis, and acid reflux can mimic peptic ulcers.
Causes and Risk Factors
Common Causes of Stomach Ulcers:
- Helicobacter pylori (H. pylori) infection
- Long-term use of NSAIDs (e.g., ibuprofen, aspirin)
- Excessive alcohol consumption
- Smoking
- Severe stress
Can Stress Cause an Ulcer? While stress alone is not a primary cause, it can exacerbate existing conditions and delay healing.
Common Signs of Gastritis:
- Similar to ulcer symptoms, including upper abdominal pain and bloating
- Gastritis pain is often localized in the upper abdomen
Difference Between Gastritis and Ulcers: Gastritis is inflammation of the stomach lining, while ulcers are sores that penetrate through the stomach lining. Both conditions share similar symptoms but require different treatments.
Treatment Options for Stomach Ulcers
Dietary Changes
Adopting a diet that includes foods that are gentle on the stomach and avoiding those that can exacerbate ulcers. Recommended dietary changes include:
- Eating smaller, more frequent meals instead of large meals.
- Avoiding spicy, acidic, or fried foods.
- Incorporating foods that promote healing, such as fiber-rich fruits and vegetables, lean proteins, and whole grains.
- Using supplements like ColoFlax to support digestive health.

Reduces irritation of the stomach lining, helps manage symptoms, and promotes healing of the ulcer. Dietary adjustments can also prevent recurrence by maintaining a healthy digestive environment.
Symptom relief can occur within a few weeks of dietary changes, but ongoing adherence to dietary recommendations is necessary for long-term management.
Medications
Use of various medications to reduce stomach acid, promote healing, and eliminate the bacteria causing the ulcers. Common medications include:
- Proton Pump Inhibitors (PPIs): Reduce stomach acid production (e.g., omeprazole, esomeprazole).
- H2-Receptor Antagonists: Decrease acid production (e.g., ranitidine, famotidine).
- Antacids: Neutralize existing stomach acid (e.g., magnesium hydroxide, aluminum hydroxide).
- Antibiotics: Eradicate H. pylori infection if present (e.g., amoxicillin, clarithromycin).
- Cytoprotective Agents: Protect the stomach lining (e.g., sucralfate, misoprostol).

Reduces stomach acid, alleviates pain, promotes healing of the ulcer, and eradicates H. pylori infection. Medications help manage symptoms and prevent complications.
Symptom improvement is often seen within days to weeks, with full healing typically occurring within 4-8 weeks. The course of antibiotics usually lasts 1-2 weeks.
Vagotomy
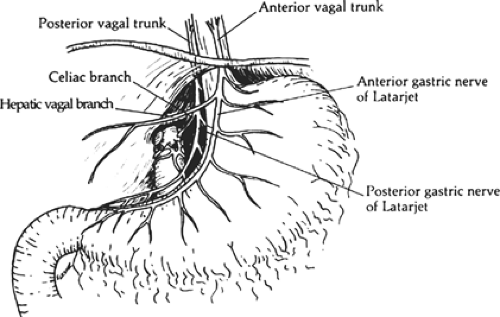
Vagotomy involves cutting the vagus nerve to reduce acid secretion in the stomach. This procedure can be performed using minimally invasive laparoscopic techniques. The vagus nerve controls acid production by stimulating the stomach's parietal cells. By cutting specific branches of this nerve, acid secretion is significantly reduced, thereby allowing the ulcer to heal.
- Reduces Acid Production: Decreases the amount of acid produced by the stomach, which helps in healing the ulcer and preventing new ulcers from forming.
- Promotes Healing: By reducing acid levels, the stomach lining can heal more effectively, and symptoms such as pain and discomfort are alleviated.
- Prevents Recurrence: Particularly beneficial for patients whose ulcers do not respond to medication.
- Hospital Stay: Typically requires a hospital stay of a few days.
- Full Recovery: Complete recovery usually takes several weeks. Patients will need to gradually return to normal activities and follow a specific diet to aid in recovery.
- Follow-Up Care: Regular follow-up appointments to monitor healing and manage any potential side effects.
Partial Gastrectomy

Partial gastrectomy involves the surgical removal of a portion of the stomach. The procedure is aimed at removing the part of the stomach that contains the ulcer. The remaining portions of the stomach are then reconnected to maintain the continuity of the digestive tract. This procedure is often used when ulcers are recurrent or complicated by bleeding, perforation, or obstruction.
- Effective Ulcer Removal: Directly removes the ulcer and any surrounding damaged tissue, which is crucial for ulcers that have not healed with medication.
- Reduces Acid Production: By removing part of the stomach that produces acid, overall acid levels in the stomach are reduced.
- Improves Quality of Life: Alleviates severe symptoms and prevents further complications, significantly improving the patient's quality of life.
- Hospital Stay: Typically ranges from a few days to over a week, depending on the extent of the surgery.
- Full Recovery: Patients can expect full recovery within several weeks. This includes careful monitoring of nutritional intake and gradual reintroduction of normal foods.
- Post-Surgery Care: Involves dietary adjustments and possibly vitamin supplements to ensure proper nutrition due to reduced stomach size.
Frequently Asked Questions (FAQs)
Burning stomach pain, feeling of fullness, bloating, belching, heartburn, and nausea.
Abdominal pain, frequent burping, loss of appetite, unintentional weight loss, and bloating.
Dark or tarry stools indicating bleeding.
A burning pain in the upper abdomen.
Typically felt in the upper abdomen and can be described as burning or gnawing.
Yes, symptoms can include nausea and vomiting.
Ulcer pain can be constant or intermittent.
Yes, urgent care can diagnose a stomach ulcer through various tests.
Blood tests can detect H. pylori infection but not the ulcer itself.
Ulcer pain is typically more persistent and severe than acid reflux, which is more commonly associated with heartburn.
A CT scan can detect complications like perforations but is not the primary diagnostic tool for ulcers.
GI doctors use endoscopy to directly visualize the ulcer.
Symptoms, blood tests, stool tests, and breath tests can suggest the presence of an ulcer.
Yes, pancreatitis can mimic ulcer symptoms.
Submit your Suggestion





