Colon polyps are abnormal growths that develop in the lining of the colon or rectum. While most polyps are benign (non-cancerous), some may develop into colorectal cancer over time if left untreated. They are often detected during routine colonoscopies.
Are Colon Polyps Cancerous?
Not all polyps are cancerous, but some types have a higher risk of turning into colorectal cancer over time.
The three main types of colon polyps are:
- Adenomatous Polyps (Adenomas) – Can develop into cancer if not removed.
- Hyperplastic Polyps – Generally benign and low risk.
- Serrated Polyps – May lead to cancer, especially if located in the upper colon.
How Serious Are Polyps in the Colon?
Most polyps are harmless, but if left untreated, some can grow larger and become cancerous over time. Early detection and removal significantly reduce colorectal cancer risk.
What Size of Colon Polyp is Worrisome?
- Small polyps (less than 5mm): Low cancer risk.
- Medium polyps (5-9mm): Require removal as a precaution.
- Large polyps (10mm+): Higher cancer risk; require immediate removal.
- Giant polyps (2cm+): Often pre-cancerous or cance
Symptoms
What Are the Symptoms of Large Polyps in the Colon?
Larger colon polyps may cause:
- Blood in the stool (bright red or dark, tarry stools).
- Persistent diarrhea or constipation lasting more than a week.
- Excessive mucus in the stool (due to irritation from the polyp).
- Iron deficiency anemia (caused by slow, undetected bleeding).
Do Colon Polyps Cause Fatigue?
Yes. If a polyp causes chronic bleeding, it can lead to iron deficiency anemia, which may result in fatigue, weakness, and dizziness.
Do Colon Polyps Make You Gassy?
In some cases, polyps can cause bloating, gas, or a feeling of incomplete bowel emptying due to their size or location.
How Do Doctors Check for Colon Polyps?
- Colonoscopy: The gold standard for detecting and removing polyps.
- Sigmoidoscopy: Examines the lower colon for polyps.
- CT Colonography (Virtual Colonoscopy): Uses imaging to detect polyps without insertion.
- Stool Tests (FIT, FOBT, or Cologuard): Can detect blood or DNA markers from cancerous polyps.
Causes and Risk Factors
Colon polyps develop due to abnormal cell growth in the colon lining, often influenced by genetic, dietary, and lifestyle factors. While many polyps remain benign, certain risk factors increase the likelihood of polyp formation and progression to colorectal cancer.
What Causes Polyps in the Colon?
Polyps form when colon cells grow and divide too quickly, leading to the development of tissue overgrowth. Some of the main causes include:
🧬 Genetic Mutations – DNA changes in colon cells trigger polyp formation.
🥩 Dietary Habits – Diets high in red and processed meats and low in fiber are linked to higher polyp risk.
🔥 Chronic Inflammation – Conditions like ulcerative colitis and Crohn’s disease can lead to polyp development.
🍺 Alcohol & Smoking – Both contribute to colon irritation and DNA damage, increasing cancer risk.
📉 Obesity & Sedentary Lifestyle – A lack of exercise is associated with slower digestion and increased inflammation.
🩺 Age & Family History – Polyps are more common after 50, and individuals with relatives who had colon polyps or colorectal cancer have a higher risk.
Are Some People More Likely to Get Colon Polyps?
Yes, certain groups have a higher risk of developing polyps:
🔹 Age 50+ – The risk of polyps increases significantly with age.
🔹 Family History – If a parent or sibling had colon polyps, your risk doubles.
🔹 Personal History of Polyps – If you’ve had a polyp before, there’s a high chance another will develop.
🔹 Inflammatory Bowel Disease (IBD) – Chronic inflammation in the colon makes polyp formation more likely.
🔹 Diabetes & Insulin Resistance – These conditions may contribute to abnormal cell growth.
Treatment Options for Colon Polyps
Treatment for colon polyps focuses on removal and prevention of recurrence. Since polyps have the potential to become cancerous, early detection and removal through routine colonoscopies are essential.
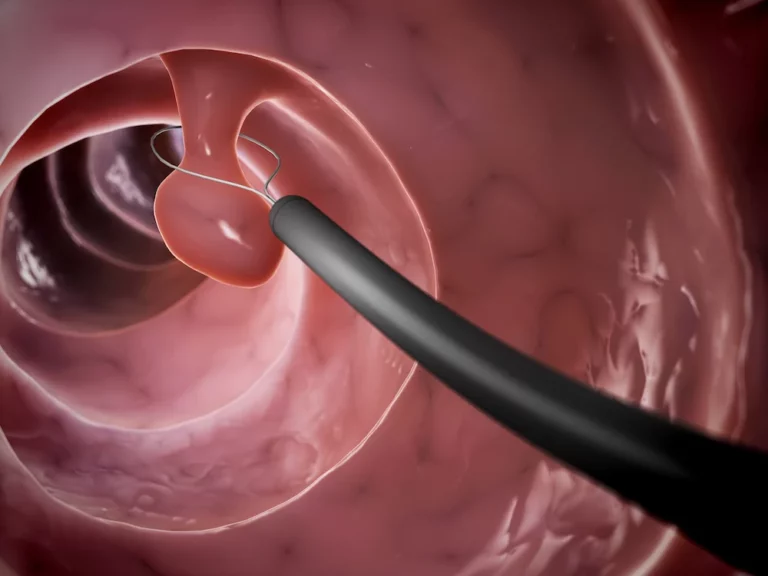
Colonoscopy & Polypectomy
A colonoscopy is a minimally invasive procedure that allows a gastroenterologist to examine the inner lining of the colon using a flexible tube equipped with a small camera. If polyps are detected, they can often be removed immediately through polypectomy—a technique that uses a wire loop or biopsy forceps to excise and retrieve the polyp for further analysis.
✅ Non-invasive removal of polyps during routine screening.
✅ Prevents cancerous transformation of precancerous polyps.
🔹 Same-day procedure with minimal downtime.
🔹 Mild bloating or gas may occur, but most patients resume normal activities within 24 hours.
Endoscopic Mucosal Resection (EMR)
EMR is a specialized endoscopic technique used for larger, flatter, or more complex polyps that cannot be removed via standard polypectomy. This technique involves lifting the polyp off the colon wall using an injected liquid solution before excising it with a snare or electrocautery.
✅ Removes larger polyps without surgery.
✅ Reduces the need for more invasive procedures.
🔹 Short recovery time, but some patients may require observation.
Surgical Polyp Removal: Colectomy
In cases where polyps are too large, exhibit cancerous changes, or carry a high risk of malignancy, surgical removal of part or all of the colon (colectomy) may be recommended. There are two main surgical approaches:
- Laparoscopic Colectomy – A minimally invasive approach where small incisions are made, and specialized instruments are used to remove the affected portion of the colon.
- Total Colectomy – This is performed in cases of hereditary conditions such as Familial Adenomatous Polyposis (FAP) or other widespread polyp syndromes. It involves the removal of the entire colon to prevent colorectal cancer.
✅ Removes polyps that cannot be extracted via colonoscopy.
✅ Prevents cancer progression in high-risk cases.
🔹 Hospital stay of a few days may be required.
🔹 Full recovery can take weeks to months, depending on the procedure.
Post-Treatment Lifestyle Adjustments
After polyp removal, lifestyle modifications play a crucial role in reducing the risk of recurrence and maintaining colon health.
How to Prevent Colon Polyps from Coming Back?
✔ Increase fiber intake – Eat at least 30g of fiber daily from whole foods or use a Fiber supplement such as ColoFlax.
✔ Maintain a healthy weight – Obesity is linked to a higher risk of polyps.
✔ Limit red & processed meats – Reduce consumption of bacon, hot dogs, and deli meats.
✔ Stay active – Engage in 150 minutes of moderate exercise weekly.
✔ Quit smoking & reduce alcohol intake – Both contribute to colon irritation and DNA damage





