Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder characterized by chronic abdominal pain, bloating, and changes in bowel habits, including diarrhea, constipation, or both. IBS is a functional disorder, meaning it affects how the gut works but doesn’t cause visible damage to the digestive tract.
Diagnosis
Symptoms:
- Abdominal pain or cramping
- Bloating and gas
- Diarrhea, constipation, or alternating between both
- Mucus in the stool
- An urgent need to have a bowel movement
Location of IBS Pain:
IBS pain is typically located in the lower abdomen but can be felt anywhere in the abdominal area. It is often described as cramping or sharp pains that can vary in intensity.
Appearance of IBS Feces:
IBS feces can vary significantly but may include:
- Loose, watery stools
- Hard, lumpy stools
- Alternating between diarrhea and constipation
- Mucus in the stool
Mucus in the stool can be a symptom of IBS due to inflammation or irritation in the intestines, which causes the production of excess mucus. White bits in poop could be undigested food, mucus, or, in some cases, parasitic infections. If this issue persists, it’s important to consult a healthcare provider. White fuzzy stuff on poop is usually mucus, indicating inflammation or irritation in the intestines often associated with IBS.

Causes and Severity
What causes IBS?
The exact cause of IBS is unknown, but several factors can contribute, including:
- Abnormal muscle contractions in the intestines
- Increased sensitivity in the digestive tract
- Inflammation in the intestines
- Severe infections, such as gastroenteritis
- Changes in gut bacteria
- Stress and anxiety
Why is my IBS getting worse as I get older?
IBS symptoms can fluctuate over time and may worsen with age due to factors like stress, dietary changes, decreased physical activity, and hormonal changes. It’s important to manage symptoms through lifestyle adjustments and medical guidance.
What is the life expectancy of someone with IBS?
IBS does not affect life expectancy. However, it can significantly impact the quality of life due to chronic symptoms. Proper management and treatment can help individuals lead a normal, healthy life.
Treatment Options for Irritable Bowel Syndrome
IBS can be managed through various methods, tailored to each individual’s symptoms and lifestyle.
Dietary Changes
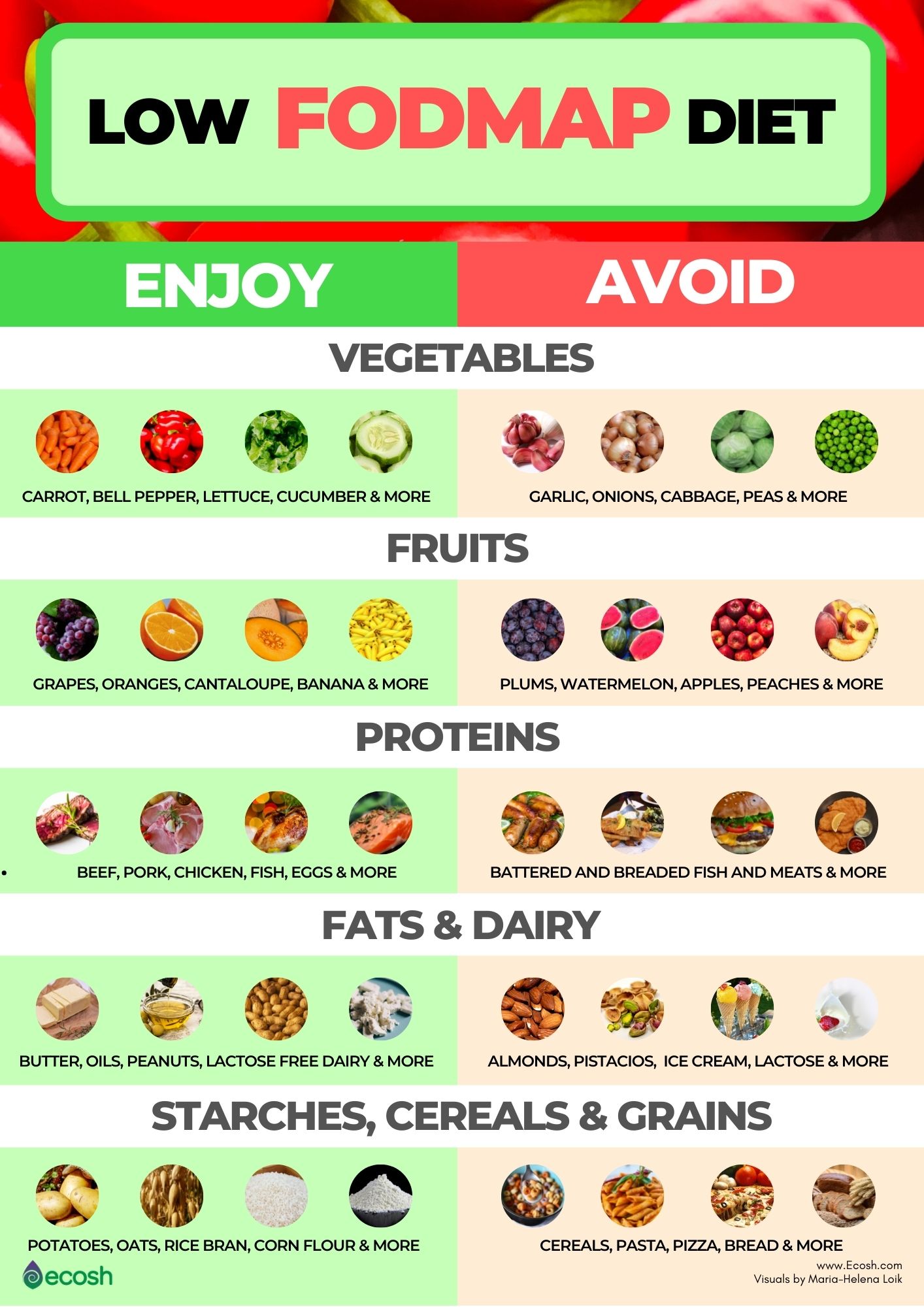
Adopting a low-FODMAP diet can help reduce symptoms. This diet involves avoiding certain carbohydrates that are poorly absorbed in the small intestine and ferment in the colon, causing gas and bloating. Supplements like ColoFlax, which combine fiber, prebiotics, and beneficial supplements, can also support digestive health.
Individuals who experience significant bloating and abdominal discomfort.
Symptoms can improve within a few weeks of starting the diet, but it requires ongoing commitment and adjustments.
Medication
Medications can help manage specific symptoms of IBS. These may include antispasmodics to reduce cramping, laxatives for constipation, or anti-diarrheal agents for diarrhea. It is essential to consult a healthcare provider to get the right prescription tailored to your needs.

Patients with moderate to severe IBS symptoms that do not respond to dietary changes alone.
Improvement can be seen within days to weeks, depending on the medication and individual response.
Frequently Asked Questions (FAQs)
A hemorrhoid can appear as a sudden onset painful lump that may be red, angry, and inflamed. Hemorrhoids can cause discomfort, swelling, rectal pain, anal discharge, and itching or irritation of the anus. These signs of hemorrhoids should not be ignored.
Watch out for these symptoms that may indicate you have hemorrhoids:
- Painful swelling
- Red marble-like growth or lump
- Sharp rectal pain
- Anal discharge
- Irritation and itching
- Rectal bleeding
Usually, symptoms last only a few days and there are plenty of effective ways to treat. Contact us for quick, painless, easy treatment for hemorrhoids – performed in-office. We offer solutions without need for surgery, except in the worst case scenarios.
ColoWell America’s gold standard RUBBER BAND LIGATION – a quick, non-surgical, in-office procedure with little to no pain or complications.
Rubber band ligation is preferred for hemorrhoids because of its effectiveness and affordability compared to other more invasive interventions and non-beneficial over-the-counter remedies.
How the treatment works:
- The treatment targets the blood vessel which feeds the hemorrhoid ligating the blood vessel and cutting off the blood supply to the hemorrhoid.
- The blood flow to the hemorrhoid is interrupted and it begins to shrink.
- Since the hemorrhoid has lost its connection with the feeding vessel, it continues to shrink and fall off during the 3-7 days following treatment.
Affordable, No time off necessary, No hospital visits. No need for special prep before procedure, Performed In Office In Minutes.
Rubber band ligation is the best treatment modality. Complications with banding are little to none. The procedure does not require surgery or a hospital visit, and you don’t have to take off work or require any difficult preparation!
To help prevent hemorrhoids and hemorrhoid recurrence you can eat more high fiber foods, including fruits, vegetables and whole grains. There are also fiber supplements like ColoFlax, Metamucil or Citrucel. Our doctor also recommends daily flax seed powder ingestion (2tbsp/day). You can also help prevent hemorrhoids by drinking four to six glasses of water a day and exercising regularly to help the bowels to move normally.
During pregnancy and delivery hemorrhoids can occur due to anal pressure, constipation, and pushing. Hemorrhoids are also commonly known as piles. It is recommended to eat fiber during pregnancy to avoid constipation, which can lead to hemorrhoidal issues. See a proctologist if you are suffering from hemorrhoids during or after pregnancy.
Internal hemorrhoids that prolapse and protrude can often cause bright red bleeding. Mostly this is painless bleeding seen on the toilet paper with wiping.
External skin tags or External hemorrhoidal tissue usually doesn’t cause bleeding. These external hemorrhoids can cause itching and problems with hygiene.
While hemorrhoids may not be cured with topical treatment, symptomatic relief from pain and itching can be obtained with over-the-counter creams such as Preparation H and Lidocaine, or prescriptions medications like Nifedipine cream.
Thrombosed hemorrhoids are blood clots in a hemorrhoid. This can result in itching around your anus, bleeding when you have a bowel movement, and swelling or lumps around the anus.
There are many causes of thrombosed hemorrhoids, including excessive straining with bowel movement when constipated, diarrhea, abnormal and irregular bowel movements, pregnancy and postpartum state, and prolonged sitting (for example, during travel, working at a desk, etc.)
We use rubber band ligation (RBL) as our standard for hemorrhoid surgery. The doctor places a small rubber band at the base of the hemorrhoid, which in result stops the blood supply and causes the hemorrhoid to shrink and fall off. A hemorrhoidectomy is another choice for hemorrhoid surgery. The procedure removes the hemorrhoid, blood clot and blood vessels. You may get partial anesthesia during this procedure and a hemorrhoidectomy is only performed for the most severe hemorrhoid cases.
How to treat hemorrhoids is based on a patient’s individual condition. Most cases require one to three appointments to prevent recurrence.
Many patients ask us: “Will the hemorrhoids go away on their own?”
The answer lies in the lifestyle choices you make following treatment.
Make FIBER a daily part of your diet. “Ground flax seed is an excellent source of fiber!” – Shiraz Farooq, MD
- Choose a plant-based diet to avoid constipation
- Be sure to drink four to six glasses of water throughout the day
- Avoid strenuous activities
Yes! Contact us to verify your eligibility for services. We also offer Self-Pay rates.
Submit your Suggestion





